Organon offers medical, prescription drug, dental and vision benefits as well as a variety of enhanced medical benefit options that provide extra support for managing medical concerns or conditions.
The Organon Preferred Provider Organization (PPO) medical plan is administered by Horizon BlueCross BlueShield (BCBS).
The Organon PPO provides a wide range of services, including doctor visits, testing, hospitalizations and emergency care. You are not required to designate a primary care physician (PCP) or seek a referral to see a specialist.
In a PPO, you can see any provider you choose, however, you will generally pay less for services when you use the extensive network of plan providers. Preventive care is fully covered in-network.
You also can decline medical coverage.
Founders who enroll for medical coverage also have access to these benefits:
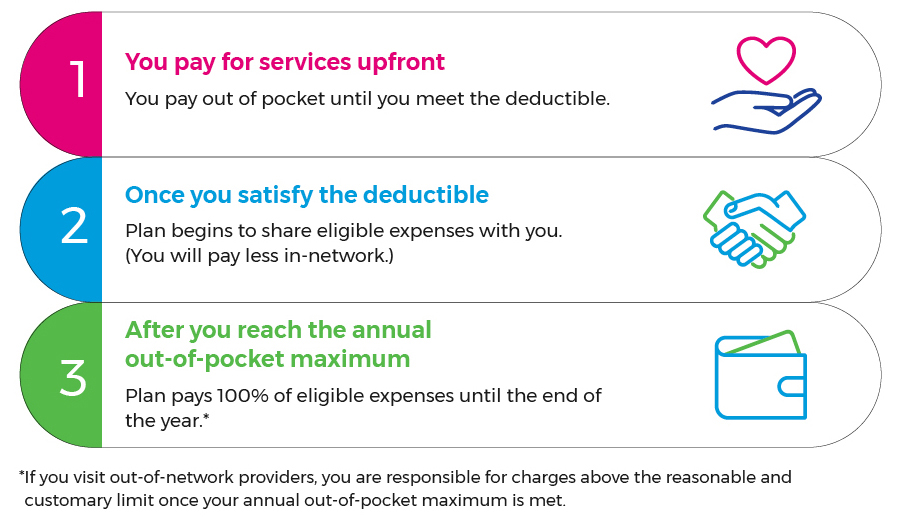
How you’ll pay for care
The Organon medical plan includes a travel and lodging benefit up to a lifetime maximum of $10,000 (for most services) to ensure you have access to medical care not available within 100 miles of your home. Contact Horizon BCBS at 1-800-544-1112 and ask to speak with a Health Guide for more information.
Click here for information on Horizon Behavioral Health.
For Organon medical plan members only
Horizon Health Guide is your one place to call, chat or email when you need help navigating the world of health care.
A Horizon Health Guide can help you:
For Organon medical plan members only
Lyra offers the full spectrum of mental health services to children and adults by blending one-on-one video sessions and personalized digital activities. With Lyra you can meet with a certified coach or licensed therapist or you can use Lyra’s self-care resources. Medical plan cost sharing applies to Lyra benefits.
Click here for more information on Lyra’s mental health services.
For Organon medical plan members only
Organon offers 2nd.MD to connect you with board-certified, leading doctors across the country for an expert second opinion via video or phone within three to five days. 2nd.MD experts can confirm a complex or rare diagnosis, weigh in on a prescribed treatment plan or provide an alternative approach.
For Organon medical plan members only
Livongo provides personalized support to you and your covered dependents diagnosed with type 1 or type 2 diabetes. There is no cost to you to use the program. It includes free, unlimited test strips, real‑time data analytics with educational support, and 24/7 personalized support through an advanced meter, mobile app and coaches.
The managed prescription drug program is administered by Express Scripts. If you elect the medical plan, you also will have prescription drug coverage. If you elect no coverage for medical, you will not receive prescription drug benefits, including Organon-brand prescription drugs.
You can look up in-network pharmacies and price medications here.
How you’ll pay for prescriptions
You pay out of pocket until you meet the annual out-of-pocket maximum. Prescriptions are only covered when purchased through in-network pharmacies or through the home delivery network.
There is no deductible to satisfy for prescriptions. You will pay either coinsurance or a copay, depending on the whether the drug is generic, Organon-brand, non-Organon brand or if the brand has a generic equivalent, as well as whether you purchase your prescriptions at a retail pharmacy or through the home delivery service.
Plan pays 100% of eligible prescription drugs until the end of the year for the person who reached the maximum.*
*If you visit out-of-network providers, you are responsible for charges above the reasonable and customary limit once your annual out-of-pocket maximum is met.
Expedited appointments and cancer treatment are available at Memorial Sloan Kettering (MSK) for employees and their families. You do not need to be enrolled in the Organon medical plan to use this service. MSK Direct is available to your immediate and extended family members.
Dental coverage is offered through MetLife’s Preferred Dental Program (PDP) Plus network, which includes dentists who have agreed to provide services at reduced fees. You can seek care in-network or out-of-network, but you will pay less in-network.
The plan provides preventive and diagnostic services, basic restorative care, major services and orthodontic services up to the annual benefit maximum. There is no annual deductible in-network.
Vision coverage is offered through Vision Service Plan (VSP). When you require vision care services, you have the choice of going to any licensed provider. There is no annual deductible to satisfy.
If you visit a VSP preferred provider, your out-of-pocket costs will generally be lower than if you visit an “open access” provider (one that doesn’t participate in the VSP network). VSP preferred providers are available nationwide at Costco, Pearle Vision and Visionworks. If you visit an open access provider, you will be responsible for paying any amounts over the fixed reimbursement paid by the plan.
Organon provides a full range of transgender-related services and procedures for those with a diagnosis of gender dysphoria.
Since only a limited number of expert medical professionals specialize in trans-care, you can use any accredited physician or provider, regardless of location or whether they accept insurance, and receive coverage as if it were in-network. This includes behavioral health therapists who specialize in transgender patients. We follow evidence-based guidelines provided by the World Professional Association for Transgender Health (WPATH).